Transgender
OVERVIEW
Transgender is a term used to explain the spectrum of gender identity and gender expression diversity. Gender identity is the internal sense of being male or female, but some individuals affirm their unique gender identity and no longer consider themselves to be either male or female. Gender expression is the expression of a gender identity through social roles, appearance and behaviors.
People who are transgender have a gender identity that differs from the sex assigned at birth. Their gender expression and behavior don't follow societal norms for birth assigned sex. This difference may lead to distress called gender dysphoria.
Treatment is available to assist people with such distress and it is individualized. What helps one person might be very different from what helps another person. This process may or may not involve a change in gender expression or body modifications. Treatment options include psychotherapy, feminization or masculinization of the body through hormone therapy and surgery and have been found to be medically necessary to alleviate gender dysphoria in many people. Health professionals recognized that while many individuals need both hormone therapy and surgery to alleviate their gender dysphoria, others need only one of these treatment options and some need neither. Often with the help of psychotherapy, some individuals integrate their transgender feelings into the gender role they were assigned at birth and do not feel the need to feminize or masculinize their body. Some patients may need hormones, a possible change in gender role, but not surgery and others may need a change in gender role along with surgery, but not hormones.
Health professionals can assist gender dysphoric individuals with affirming their gender identity, exploring different options for expression of that identity and making decisions about medical treatment options for alleviating gender dysphoria.
OVERVIEW
Transgender is a term used to explain the spectrum of gender identity and gender expression diversity. Gender identity is the internal sense of being male or female, but some individuals affirm their unique gender identity and no longer consider themselves to be either male or female. Gender expression is the expression of a gender identity through social roles, appearance and behaviors.
People who are transgender have a gender identity that differs from the sex assigned at birth. Their gender expression and behavior don't follow societal norms for birth assigned sex. This difference may lead to distress called gender dysphoria.
Treatment is available to assist people with such distress and it is individualized. What helps one person might be very different from what helps another person. This process may or may not involve a change in gender expression or body modifications. Treatment options include psychotherapy, feminization or masculinization of the body through hormone therapy and surgery and have been found to be medically necessary to alleviate gender dysphoria in many people. Health professionals recognized that while many individuals need both hormone therapy and surgery to alleviate their gender dysphoria, others need only one of these treatment options and some need neither. Often with the help of psychotherapy, some individuals integrate their transgender feelings into the gender role they were assigned at birth and do not feel the need to feminize or masculinize their body. Some patients may need hormones, a possible change in gender role, but not surgery and others may need a change in gender role along with surgery, but not hormones.
Health professionals can assist gender dysphoric individuals with affirming their gender identity, exploring different options for expression of that identity and making decisions about medical treatment options for alleviating gender dysphoria.
HOW TO KNOW IS CHILD TRANSGENDER AND HOW TO SUPPORT HIM
Most children by age 24 months recognize gender groups such as girl, woman and boy, man, and by age 3 years categorize their own gender.
How to know is child transgender while children might go through periods of insisting that they are the opposite gender of their birth sex? If childe has a desire to play with toys or to dress typically assigned to the opposite sex, girl insisting on standing up to urinate, or they continue to do so it was likely never a development phase. Some of transgender children, despite their authentic gender identity, learn to behave in ways that bring them the most reward.
If your child is transgender speak positively to himself and to others and do not shame or punish his gender expression. Allow child's access to gender-diverse friends, activities or resources. A transgender child living with supportive parents is likely to be a happier.
A social transition is a reversible step in which a child lives partially or completely in the preferred gender role by changing hairstyles, clothing, pronouns and perhaps name. It's important for parents and children to determine the extent of the transition and how to handle challenges such as which bathroom to use and whether transitioning will be continued at school or in the community.
ASSESSMENT AND TREATMENT OF CHILDREN AND ADOLESCENTS WITH GENDER DYSPHORIA
Suspected transgender children need a thorough diagnostic evaluation which includes physical exam of body and genitalia, biochemical and genetic tests, and imaging studies to obtain a diagnosis and to enable prognostic predictions and genetic counseling and start an individualized management plan.
The diagnosis and treatment of transgender children requires an approach implemented by experienced multidisciplinary team which includes gynecologist, pediatrician, geneticist, endocrinologist, pediatric urologist, radiologist, psychologist, psychiatrist and social worker.
There are differences in the developmental course and treatment approaches for gender dysphoria in children, adolescents and adults. An important difference between children and adolescents with gender dysphoria is in the proportion for whom dysphoria persists into adulthood. Gender dysphoria during childhood does not inevitably continue into adulthood, but the persistence of gender dysphoria into adulthood appears to be much higher for adolescents.
In most children gender dysphoria will disappear before or early in puberty. However, in some children these feelings will intensify and body aversion will develop or increase as they become adolescents and their secondary sex characteristics develop. Contrary to this, many adolescents and adults presenting with gender dysphoria do not report a history of childhood gender-nonconforming behaviors, therefore it may come as a surprise to parents and other family members, friends and community members when a gender dysphoria first becomes evident in adolescence.
Adolescents who experience their primary and/or secondary sex characteristics and their sex assigned at birth as inconsistent with their gender identity may be intensely distressed about it. Many gender dysphoric adolescents have a strong wish for hormones and surgery.
Mental health professionals should acknowledge the presenting concerns of children or adolescents and their families, offer a thorough assessment for gender dysphoria and any coexisting mental health concerns and educate patients and their families about therapeutic options, if needed. The psychiatric assessment should also be used to inform children or adolescents and their families about the possibilities and limitations of different treatments. This is necessary for informed consent. Correct information may alter a child’s or adolescent’s desire for certain treatment, if the desire was based on unrealistic expectations of its possibilities. Psychotherapy should focus on reducing a child’s or adolescent’s distress related to the gender dysphoria and on ameliorating any other psychosocial difficulties. For patients desiring sex reassignment, psychotherapy may focus on supporting them before, during and after reassignment.
Hormone therapy is used to alter patient’s hormone levels to match their gender identity. Treatment consists of implementing hormones to masculinize or feminize the body due to a gender dysphoria.
Surgical treatment of transgender patients with gender dysphoria is in a form of masculinizing or feminizing genitoplasty. Early mutilation genital and gonadal surgery is forbidden and it is considered as human right violation. Elective surgical reconstruction should not be performed without the individual's informed consent. Before surgery psychological and psychiatric evaluation and hormonal therapy are necessary. The mental health professional provides documentation of the patient’s personal and treatment history, progress and eligibility. Mental health professionals who recommend surgery share the ethical and legal responsibility for that decision with the surgeon. One referral from a qualified mental health professional is needed for top/breast and chest surgery (mastectomy, chest reconstruction or augmentation mammoplasty). Two referrals from qualified mental health professionals, who have independently assessed the patient, are needed for bottom/genital surgery (hysterectomy/salpingo-oophorectomy, orchiectomy, genital reconstructive surgeries).
PHYSICAL INTERVENTIONS FOR ADOLESCENTS
Before any physical interventions are considered for adolescents, extensive exploration of psychological, family and social issues should be undertaken. Physical interventions are divided into three categories: fully reversible interventions, partially reversible interventions and irreversible interventions.
Fully reversible interventions involve the use of GnRH analogues in adolescents to suppress estrogen or testosterone production and consequently delay the physical changes of puberty. Adolescents may be eligible for puberty suppressing hormones as soon as pubertal changes have begun. Puberty suppressing hormones gives adolescents more time to explore their gender issue and their use may facilitate transition by preventing the development of sex characteristics that are difficult or impossible to reverse if adolescents want sex reassignment. Puberty suppression may continue for a few years, at which time a decision is made to either discontinue all hormone therapy or transition to a feminizing or masculinizing hormone regimen. Pubertal suppression does not inevitably lead to social transition or to sex reassignment.
Partially reversible interventions include hormone therapy to masculinize or feminize the body. Adolescents may be eligible to begin feminizing or masculinizing hormone therapy, preferably with parental consent. In many countries 16-year-olds are legal adults for medical decision making and do not require parental consent. Preferably, treatment decisions should be made among the adolescent, the family and the treatment team.
Irreversible interventions are surgical procedures. Genital surgery should not be carried out until patients reach the legal age to give consent for medical procedures in a given country and patients have lived continuously for at least 12 months in the gender role that is congruent with their gender identity.
A staged process is recommended and moving from one stage to another should not occur until there has been adequate time for adolescents and their parents to assimilate fully the effects of earlier interventions.
HORMONE THERAPY
Feminizing or masculinizing hormone therapy, consisting of the administration of exogenous endocrine agents to induce feminizing or masculinizing changes, is a medically necessary intervention for many patients with gender dysphoria. Hormone therapy must be individualized based. Hormone therapy is a recommended criteria for some, but not all surgical treatments for gender dysphoria.
Initiation of hormone therapy may be undertaken after a psychosocial assessment has been conducted and informed consent has been obtained by a qualified health professional. Obtaining informed consent for hormone therapy is an important task to ensure that patients understand the psychological and physical benefits and risks of hormone therapy, as well as its psychosocial implications. Comprehensive information must be provided about all aspects of the hormone therapy, including both possible benefits and risks and the impact on reproductive capacity. Endocrinologists recommending the hormones should have the knowledge and experience to assess gender dysphoria.
In rare cases, hormone therapy may be contraindicated due to serious individual health conditions and in these circumstances a qualified mental health professional should assist these patients.
Feminizing or masculinizing hormone therapy will induce physical changes that are more congruent with a patient’s gender identity. In female to male patients (FtM) the following physical changes are expected to occur: deepened voice, variable clitoral enlargement, growth in facial and body hair, cessation of menses, atrophy of breast tissue, and decreased percentage of body fat compared to muscle mass. In male to female patients (MtF) the following physical changes are expected to occur: variable breast growth, decreased erectile function, decreased testicular size, and increased percentage of body fat compared to muscle mass.
Most physical changes, whether feminizing or masculinizing, occur over the course of two years. The amount of physical change and the exact timeline of effects can be highly variable.
MASCULINIZING HORMONE THERAPY
Masculinizing hormone therapy is used to alter hormone levels to match gender identity of transgender person. This therapy is not for all transgender men. People who seek masculinizing hormone therapy experience gender dysphoria, distress due to a difference between expressed gender and sex assigned at birth.
Masculinizing hormone therapy is used to induce the physical changes in body caused by male hormones (secondary sex characteristics) to promote the matching of person’s gender identity and body.
During therapy, the male hormone testosterone is given. Testosterone suppresses menstrual cycles and decreases the production of estrogen from ovaries.
Therapy is not indicated if transgender person had or have a hormone sensitive cancer, has a thromboembolic disease, is pregnant or has uncontrolled mental health issues.
Fertility and sexual function
Masculinizing hormone therapy can affect fertility and sexual function and cause other health problems. The risk of permanent infertility increases with hormones long term use. Ovarian and uterine function might not recover well enough to ensure that person can become pregnant even after discontinuation of hormone therapy. While having hormonal therapy transgender person is still at risk of pregnancy if uterus and ovaries are preserved, so contraception or an intrauterine device is necessary.
If transgender person wants to have biological children cryopreservation of mature oocyte is needed.
Health evaluation
Before starting masculinizing hormone therapy complete health evaluation is mandatory (review of medical history, physical exam, laboratory tests, pregnancy test). Mental health evaluation needs to be provided by expertise in transgender health.
Therapy
Testosterone is given by injection or a patch or gel applied to the skin.
Body changes
Therapy will begin producing body changes within weeks to months. Oily skin and acne will begin one to six months after treatment with maximum effect within one to two years. Cessation of period will occur within two to six months of treatment. Voice deepening will begin three to 12 months after treatment with maximum effect within one to two years. Facial and body hair growth will begin three to six months after treatment with maximum effect within three to five years. Body fat redistribution will begin within three to six months with maximum effect within two to five years. Clitoral enlargement and vaginal atrophy will begin three to six months after treatment with maximum effect within one to two years. Increased muscle mass and strength will begin within six to 12 months after treatment with maximum effect within two to five years. Scalp hair loss will occur within 12 months of treatment.
Complications
Complications of masculinizing hormone therapy are: acne, male baldness, weight gain, sleep apnea, polycythemia (producing too many red blood cells), elevated liver function tests, dyslipidemia (an abnormal amount of lipids in the blood), hypertension (high blood pressure), type 2 diabetes, cardiovascular disease and worsening of psychotic condition.
Follow up
After masculinizing hormone therapy breast and cervical cancer screening (doctor must know for testosterone therapy due to cervical atrophy and cervical dysplasia caused by therapy) and evaluation for obstructive sleep apnea are needed.
FEMINIZING HORMONE THERAPY
Feminizing hormone therapy is used to alter hormone levels to match gender identity of transgender person. This therapy is not for all transgender women. People who seek feminizing hormone therapy experience gender dysphoria, distress due to a difference between expressed gender and sex assigned at birth.
Feminizing hormone therapy is used to induce the physical changes in body caused by female hormones (secondary sex characteristics) to promote the matching of person’s gender identity and body.
During therapy, the hormone estrogen and medication to block hormone testosterone are given. Estrogen decreases testosterone production and induces feminine secondary sex characteristics.
Therapy is not indicated if transgender person had or have a hormone sensitive cancer (prostate cancer), has a thromboembolic disease or has uncontrolled mental health issues.
Fertility and sexual function
Feminizing hormone therapy can affect fertility and sexual function and cause other health problems. The risk of permanent infertility increases with hormones long term use. Testicular function might not recover well enough to ensure conception even after discontinuation of hormone therapy.
If transgender woman wants to have biological children sperm cryopreservation is needed before starting therapy.
Health evaluation
Before starting feminizing hormone therapy complete health evaluation is mandatory (review of medical history, physical exam, laboratory tests). Mental health evaluation needs to be provided by expertise in transgender health.
Therapy
Feminizing hormone therapy begins by taking the diuretic spironolactone daily to block androgen (male sex hormone) receptors and suppress testosterone production. After six to eight weeks estrogen is administrated to decrease testosterone production and induce feminization.
Estrogen is given by injection or in skin preparations (cream, gel, spray or patch).
Progesterone can be used as additional drug to improve breast development and finasteride or topical minoxidil or both for people prone to male-pattern baldness.
Body changes
Therapy will begin producing body changes within weeks to months. Decreased libido will begin one to three months after starting treatment with maximum effect within one to two years. Decreased spontaneous erections will begin one to three months after treatment with maximum effect within three to six months. Slowing of scalp hair loss will begin one to three months after treatment with maximum effect within one to two years. Softer, less oily skin will begin three to six months after treatment. Testicular atrophy will begin three to six months after treatment with maximum effect within two to three years. Breast development will begin three to six months after treatment with maximum effect within two to three years. Redistribution of body fat will begin three to six months after treatment with maximum effect within two to five years. Decreased muscle mass will begin three to six months after treatment with maximum effect within one to two years. Decreased facial and body hair growth will begin six to 12 months after treatment with maximum effect within three years.
Complications
Complications of feminizing hormone therapy are: deep vein thrombosis or pulmonary embolism (a blood clot in a deep vein or in a lung), high triglycerides (type of fat) in blood, gallstones, weight gain, elevated liver function tests, decreased libido, erectile dysfunction, infertility, hyperkalemia (high blood levels of potassium), hypertension (high blood pressure), type 2 diabetes, cardiovascular disease, hyperprolactinemia (high blood levels of prolactin) or prolactinoma (noncancerous tumor, adenoma of the pituitary gland in brain, overproduces the hormone prolactin).
Follow up
After feminizing hormone therapy breast cancer screening, calcium and vitamin D supplementation and prostate cancer screening are necessary. With estrogen treatment PSA (prostate specific antigen) is expected to decrease by 50 percent.
GENDER AFFIRMING SURGERY
Gender affirming surgery changes a person’s sexual characteristics to better reflect their gender identity. World Professional Association for Transgender Health (WPATH) have established Standards of Care that apply before someone can apply for and receive gender affirming surgery (https://www.wpath.org/publications/soc).
Gender affirming surgeries include masculinization or feminization procedures. These procedures are categorized as genital and non-genital (facial, chest, etc) surgery.
Surgery, particularly genital, is often the last and the most considered step in the treatment process for gender dysphoria. While many patients find comfort without surgery, for many others surgery is essential and medically necessary to alleviate their gender dysphoria.
Surgeons who perform gender affirming operations for gender dysphoria should be board certified urologists, gynecologists, plastic or general surgeons. They should regularly attend professional meetings where new techniques are presented. Surgeons should be experienced in more than one surgical technique for genital reconstruction so that they can offer and choose the ideal technique for each patient. If a surgeon is skilled in a single technique and this procedure is either not suitable for or desired by a patient, the surgeon should inform the patient about other procedures and offer referral to another appropriately skilled surgeon. The internet is often effectively used by patients to share information on their experience with surgeons and their teams.
A criteria for gender affirming surgeries is documentation of persistent gender dysphoria by two qualified mental health professionals. For some surgeries, additional criteria include preparation and treatment consisting of feminizing or masculinizing hormone therapy and one year of continuous living in a gender role that is congruent with patient’s gender identity. When patients with gender dysphoria are also diagnosed with severe psychiatric disorders an effort must be made to improve these conditions with psychotropic medications and/or psychotherapy before surgery is planned. After conducted treatment reevaluation by a mental health professional should be performed prior to surgery. No surgery should be performed while a patient is actively psychotic.
Surgeons must have insight into each patient’s history and must talk with them and have close working relationships with other health professionals who have been actively involved in patient’s clinical care. Once a surgeon is satisfied that the criteria for specific surgery have been met, surgical treatment should be considered and a preoperative surgical consultation should take place. During this consultation, the procedure and postoperative course should be extensively discussed with the patient. Surgeons will discuss about the different surgical techniques available, the advantages and disadvantages of each technique, the limitations of a procedure to achieve ideal results and the inherent risks and possible complications of the various techniques.
These discussions are the core of the informed consent process, which is both an ethical and legal requirement for any surgical procedure. Ensuring that patients have a realistic expectation of outcomes is important in achieving a result that will alleviate their gender dysphoria. All of this information should be provided to patients in writing in a native language or in which they are fluent. Patients should receive the information in advance and be given plenty of time to analyze it carefully. Because these surgeries are irreversible, care should be taken to ensure that patients have sufficient time to analyze and understand information fully before they are asked to provide informed consent.
MASCULINIZING SURGERY
Masculinizing surgery is often chosen as a final step in the process of treating gender dysphoria due to a difference between expressed gender and sex assigned at birth.
Surgery includes:
- Mastectomy, removal of breasts
- Salpingo-oophorectomy and total hysterectomy, removing of uterus and cervix, and fallopian tubes and ovaries
- Vaginectomy, removing all or part of vagina
- Metoidioplasty, increasing the length of the clitoris or phalloplasty, creating a neopenis
- Urethroplasty, creating of male urethra
- Scrotoplasty, creating a scrotum
- Implantation of testis prosthesis.
- Implantation of penile implants
It can also include placement of pectoral implants to create the appearance of a defined male chest and aesthetic procedures to remove fat from specific areas of the body (liposuction) or fat grafting.
Masculinizing surgery is not for all transgender men, but only for those with gender dysphoria. For them masculinizing surgery is a natural step important to their sense of self. However, many do not choose to have surgery.
Contraindications
Surgery is not indicated if trans man (female to male, FtM) has unmanaged mental health conditions, heart or kidney disease, a bleeding disorder or a history of deep vein thrombosis or pulmonary embolism (a blood clot in a deep vein or in a lung).
Fertility
Masculinizing surgery can harm or end fertility. If transgender person wants to have biological children cryopreservation of mature oocyte is needed.
What is necessary before surgery?
Before surgery, consulting of a board certified surgeon who is experienced in the procedures is necessary. Surgeon will provide all necessary informations about preoperative preparation, describe surgery options and potential results, risks and follow up and the kind of follow-up procedures that might be necessary.
Before starting surgery complete health evaluation is mandatory (review of medical history, physical exam, laboratory tests, pregnancy test).
Mental health evaluation needs to be provided by expertise in transgender health. Before having a mastectomy, hysterectomy, salpingo-oophorectomy and vaginectomy, metoidioplasty or phalloplasty it is required to obtain two letters of support from a mental health provider competent in transgender health.
Prior to surgical intervention (hysterectomy and salpingo-oophorectomy) the hormone therapy need to be conducted. The aim of hormone therapy prior to these procedures is to introduce a period of reversible estrogen suppression before undergoing irreversible surgical intervention.
Trans-man might consider talking to others who have had masculinizing surgery before taking this step to shape expectations of what can be achieved by this kind of surgery and to have insight on what personal and social problems they might experience during treatment.
After thoroughly discussion about the risks, benefits, cost, alternatives, social and legal implications, potential complications, impact on sexual function and fertility, procedure irreversibility the informed consent is necessary.
Chest surgery
Masculinizing chest surgery involves the removal of breast tissue (mastectomy) and it is done at the hospital under general anesthesia. After the procedure patient goes home the same day. Some breast tissue will likely remain regardless of the surgical technique so routine breast cancer screening is necessary.
The chest surgery involves several procedures.
Liposuction
Chest will be liposuctioned with or without small incision to reduce nipple or areolar size. After the procedure compression garment is necessary.
Periareolar surgery
An incision is made around nipple areolar complex and all of the tissue underneath is removed. After the procedure the nipple areolar complex is sutured with resorbable sutures that will dissolve on their own and compression garment is necessary.
Double incision with free nipple grafts
An incision below the breast is made and all excess tissue is removed. Then the nipple areolar complex is grafted onto the chest wall. After the procedure drains and compression garments are necessary.
Recovery time and resuming of normal activities
After surgery patient could experience some discomfort, swelling and bruising, which can be minimized with rest and pain medications. Drains are removed on the third day of surgery. Patient will continue to wear compression garment for three weeks, except when showering. After four weeks most patients are ready to return to all activities.
Complications of top surgery
When the amount of breast tissue removed requires skin removal a scar will result and the patient should be informed about it. Complications of subcutaneous mastectomy can include nipple necrosis, contour irregularities and unpleasant scarring.
GENITAL SURGERY
Total hysterectomy, salpingo-oophorectomy and vaginectomy
Total hysterectomy with salpingo-oophorectomy is a procedure in which the uterus, cervix, ovaries and fallopian tubes are removed. There are multiple techniques for hysterectomy: laparoscopic, abdominal and vaginal and they are performed by gynecologists.
Vaginectomy is a procedure of removing all or part of vagina. Vaginectomy is done through colpoclesis, consisting of ablation of the vaginal epithelium with electrocautery followed by closure of the vaginal lumen and drain placement.
Hysterectomy with salpingo-oophorectomy results in irreversible reproductive sterilization. It can be performed as a separate procedure or simultaneously with metoidioplasty or phalloplasty.
Metoidioplasty
Metoidioplasty is a procedure to create a phallus by increasing the length of the clitoris using a genital tissue. Metoidioplasty takes advantage of enlarging effect of testosterone on the clitoris and results in a small phallus. The length of phallus is dependent on how much clitoral growth testosterone has caused. Because of the small size of phallus best result can be achieved if patients are close to their ideal weight before surgery.
Before procedure a vaginectomy need to be performed to create an anatomically male perineum. The testosterone enlarged clitoris is freed from labia minora and a suspensory ligament.
Urethra needs to be extended through released clitoris using a buccal mucosa graft (typically taken from the lining of patient’s mouth) and genital flaps. Genital tissue is wrapped around the released clitoris to transform it into a phallus. Scrotoplasty and insertion of testicular implants is done during the operation. All these steps of metoidioplasty procedure can be performed in one stage (clitoral release, urethral lengthening, scrotoplasty, insertion of testicular implants, vaginectomy with perineoplasty)
After metoidioplasty, a tube placed in urethra and suprapubic bladder catheter to collect urine are necessary. Recovery might take up to two-three weeks.
This procedure will make standing voiding possible. A penis created by this procedure has length of between 3 and 8 cm, but full sensation and orgasmic function are retained. Metoidioplasty does not produce obvious surgery scars. Penetration probably will not be possible because of small phallus. If a patient wants penetrative intercourse, the total phalloplasty with penile implants, as staged procedures, needs to be performed.
Many patients will benefit from a plastic surgery procedure called pubic lift or mons resection. In this procedure fat from the pubic mound is removed and the phallus is pulled into a higher, more natural-looking position.
Complications of procedure include migration and/or extrusion of testicular implants, urethral fistula or stricture, infection.
Recovery time and resuming of normal activities
After surgery patient could experience some discomfort, swelling and bruising, which can be minimized with rest and pain medications. Daily medical check-ups are necessary. After four to six weeks most patients are ready to return to all activities.
Phalloplasty (total phalloplasty)
Phalloplasty is a procedure to create a neopenis using an extragenital tissue. The final goal of phalloplasty is male appearance of genitals with full sexual and voiding function. Typically, penetrative sexual intercourse and voiding in standing position could be achieved in three stages. First stage is creating of the neophallus (with or without vaginectomy and hysterectomy), second stage is urethral join-up, scrotoplasty with testicular implant and glansplasty; and finally, third stage is insertion of penile prosthesis. Some steps in these stages may differ.
Surgical procedures used for creating a neophallus are divided into pedicle flaps and free flaps. Pedicle flaps are used from the thigh, groin or lower abdomen and free flaps involve transfer of tissue from a remote location, such as forearm or patients back (latissimus dorsi), and microsurgical anastomosis with vessels and nerves at the recipient site.
Grafted tissue and skin from other parts of the body will be rolled into the shape of a penis and anchored into proper position. Also, urethral lengthening trough neopenis, grafting of nerves and blood vessels to provide sensation in neopenis are needed. Glansplasty (creating the penile glans), scrotoplasty and insertion of testicular implants are done during same or the following operation. Before procedure a vaginectomy (and hysterectomy, if not done previously) need to be performed to create an anatomically male perineum. These procedures cause significant scarring (contrary to metoidioplasty), particularly at the donor site of the flap.
Radial forearm free flap phalloplasty
The radial forearm free flap is the most often used technique for phalloplasty. Forearm skin with subcutaneous tissue (including radial artery, venae comitantes, cephalic vein, lateral and medial antebrachial cutaneous nerves) is used to create the phallus and urethra. Constructing a neourethral tube over catheter and multiple layer closure of neourethral tube is completed on forearm by “tube within a tube” technique. Also, neoglans could be created simultaneously by folding back wings over a de-epithelialized portion of shaft of the phallus, while phallus is steel attached to forearm blood vessels. After de-attaching of the created phallus with neourethra from forearm donor site microsurgical skills are necessary to create anastomosis between blood vessels and nerves of thigh recipient site. The dorsal clitoral nerves and the femoral artery and veins needs to be identified for micro-anastomosis. Procedure is the single stage and allows a sensate phallus and glans penis. The disadvantage of procedure is the visibility of the donor site on the forearm, limited volume of the neophallus and high rate of urethral complications (urethral stenosis and fistulas). Urethral join-up and insertion of penile implants are performed in following stages.
Latissimus dorsi musculocutaneous flap phalloplasty
Latissimus dorsi musculocutaneous flap phalloplasty with urethral lengthening consists of creating a neophallus using part of skin from patients back with part of muscle latissimus dorsi. The flap is harvested from non-dominant side and tubularized. Microvascular anastomosis is created between thoraco-dorsal vessels and femoral artery and saphenous vein. After neophallus is positioned adequately the creation of neourethra is performed by combining genital flaps. The clitoris is fixed to the ventral base of the neophallus.
The advantages of procedure are acceptable cosmetic outcome (the donor site scar is less visible and more easily concealed), good volume of neophallus, and voiding while standing. The main disadvantage is less sensitive phallus and thick skin on the neophallus. There is high rate of urethral complications (urethral stenosis and fistulas), as in all phalloplasty procedures. Creating of glans and insertion of penile implants are performed in following stages.
Abdominal phalloplasty
Abdominal phalloplasty is a one-stage procedure which results in an adult-sized phallus. Procedure uses a pedicled abdominal flap that is tubed to create the phallus. The lower abdominal arteries, veins and nerves are preserved in the flap, providing good blood supply, tactile and temperature sensation. There is a scar after procedure across the pelvis. The advantage of the procedure is less demanding surgery since there is no need for microvascular anastomosis, but the neophallus is sometimes smaller and cannot fit the penile implant.
After phalloplasty
After phalloplasty, a tube placed in urethra and suprapubic bladder catheter to collect urine are necessary, for two and three weeks respectively. After surgery patient could experience some discomfort, swelling and bruising, which can be minimized with rest and pain medications. Daily medical check-ups are necessary. After six to 12 weeks most patients are ready to return to all activities.
A penile implant will be needed in following stage to enable penetrative sexual intercourse, because neopenis is not erectile.
Many patients will benefit from a plastic surgery procedure called pubic lift or mons resection. In this procedure fat from the pubic mound is removed and the phallus is pulled into a higher, more natural-looking position.
Phalloplasty carries a high rate of complications and might require many follow-up surgical procedures. Complications can include tissue necrosis, migration and/or extrusion of testicular implants; infection.
Scrotoplasty and testis prosthesis implantation
Scrotoplasty is a surgical procedure to create a scrotum using a labia minora skin. Silicone testicular implants can be inserted simultaneously or in following surgical step.
Complications of FtM genital surgery
FtM surgical procedures are huge operations that carry a risk of minor or major complications. Some of them are related to phalloplasty (total or partial flap loss, bleeding, blood cloth, severe scarring of donor site), some of them are related to urethral lengthening (neourethral strictures and fistulas) and some of them are related to testicular or penile implants (infection, rejection, malfunction). Other complications are: an adverse reaction to anesthesia, poor wound healing, seroma (accumulation of fluid beneath the skin), hematoma (solid swelling of clotted blood within tissues), changes in skin sensation (persistent pain, tingling, reduced tactile or orgasmic sensation), tissue necrosis (dead body tissue), deep vein thrombosis or pulmonary embolism (a blood clot in a deep vein or in a lung).
Gender affirming surgical procedures significantly improve quality of life and reduce the symptoms of gender dysphoria, with low rates of regret following these gender affirming surgeries. Even patients who develop severe surgical complications seldom regret having undergone surgery.
All these procedures are performed according to WPATH Standards of Care.
FEMINIZING SURGERY
Feminizing surgery is often chosen as a step in the process of treating gender dysphoria due to a difference between expressed gender and sex assigned at birth.
Surgery includes:
- Breast augmentation, increasing the size of breasts
- Orchiectomy, removing testicles
- Vaginoplasty, creating a vagina.
To create a more feminine appearance it can also include facial procedures or body-contouring procedures.
Feminizing surgery is not for all transgender women, but only for those with gender dysphoria. For them feminizing surgery is a natural step important to their sense of self. However, many do not choose to have surgery.
Contraindications
Surgery is not indicated if trans woman (male to female, MtF) has unmanaged mental health conditions, heart or kidney disease, a bleeding disorder, or a history of deep vein thrombosis or pulmonary embolism (a blood clot in a deep vein or in a lung).
Fertility
Feminizing surgery can harm or end fertility. If transgender person wants to have biological children sperm cryopreservation is needed.
What is necessary before surgery?
Before surgery, consulting of a board certified surgeon who is experienced in the procedures is necessary. Surgeon will provide all necessary informations about preoperative preparation, describe surgery options and potential results, risks and follow up and the kind of follow-up procedures that might be necessary.
Before starting surgery complete health evaluation is mandatory (review of medical history, physical exam, laboratory tests).
Mental health evaluation needs to be provided by expertise in transgender health. Before having a breast augmentation, orchiectomy, vaginoplasty or facial feminization surgery it is required to obtain two letters of support from a mental health provider competent in transgender health.
Prior to surgical intervention (breast augmentation and orchiectomy) the hormone therapy need to be conducted. The aim of hormone therapy prior to these procedures is to maximize breast growth in order to obtain better results and introduce a period of reversible testosterone suppression before undergoing irreversible surgical intervention.
Trans-woman might consider talking to others who have had feminizing surgery before taking this step to shape expectations of what can be achieved by this kind of surgery and to have insight on what personal and social problems they might experience during treatment.
After thoroughly discussion about the risks, benefits, cost, alternatives, social and legal implications, potential complications, impact on sexual function and fertility and procedure irreversibility the informed consent is necessary.
Chest surgery
Breast augmentation
Breast augmentation is a surgical procedure to increase breast size and involves implants, fat grafting or both. If feminizing hormone therapy has not made breasts large enough, an initial surgery to place tissue expanders in front of chest muscles is needed. Every few weeks a small amount of saline injected into the tissue expanders will slowly stretch chest skin and other tissues to make room for the implants.
The implant may be placed submusculary and subglandulary. Submuscular position is between the chest muscle and rib cage, and is often used in small-breasted women. It provides extra padding, creating a natural look while decreasing potential scarring. Subglandular position is in front of the pectoral muscle and under the breast tissue, and is used in large-breasted women.
There are three types of incisions used for inserting breast implants: the inframammary, around the areola (Figure 1), and the axillary. The most used is the inframammary incision which is made under the breast and naturally hides the scar.
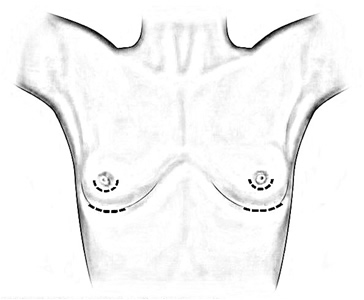
Figure 1 Breast augmentation incisions
Brest augmentation is done in general anesthesia. After the incision, in most cases the inframammary, a pocket is made behind each breast (submuscular or subglandular). The breast implants are placed in these pockets and positioned for optimal appearance and symmetry (Figure 2). All sutures are under the skin.
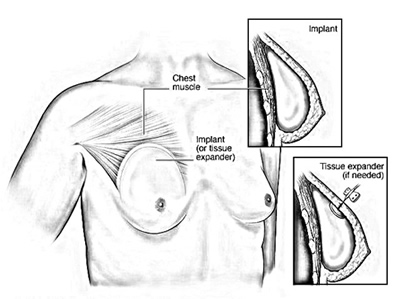
Figure 2 Placement of breast implants or tissue expanders
Most breast implants will last a lifetime, some implants may to be replaced after about 10 years.
Recovery time and resuming of normal activities
After surgery patient could experience some discomfort, swelling and bruising, which can be minimized with rest and pain medications. Most patients can do light daily activities the day after surgery. It is advised to avoid stretching and heavy lifting during the first seven to 10 days. You can return to non-strenuous work within three to seven days. Driving is possible after a week. Most swelling, bruising and soreness is gone within four to six weeks. After six to eight weeks most patients are ready to return to all activities. Final bra size can be determined within 10 to 12 weeks.
Complications of breast surgery
Rare complications of augmentation mammoplasty in MtF patients are infections and capsular fibrosis.
Facial feminization surgery and tracheal shave
Facial feminization surgery includes plastic surgery techniques to create a more feminine appearance (alter jaw, chin, cheeks, forehead, nose, areas surrounding the eyes, ears or lips). A tracheal shave is a procedure to reduce and reshape the thyroid cartilage through a small neck incision.
Most procedures are done under general anesthesia in the hospital in a form of one day surgery.
Recovery time and resuming of normal activities
After surgery patient could experience some discomfort, swelling and bruising, which can be minimized with rest and pain medications. Recovery times vary with procedures. Resting and relaxing is necessary for the first week after the surgery. Patient can go back to non-strenuous work in one to two weeks. After four weeks most patients are ready to return to all activities.
Genital surgery
Orchiectomy
Orchiectomy is a surgery procedure of removing testicles. After orchiectomy there is no need to use testosterone blockers and the amount of estrogen needed to achieve and maintain desired appearance is reduced. In most cases procedure is done as part of the surgery for vaginoplasty.
Vaginoplasty
Vaginoplasty is a surgical procedure of creating a neovagina that is functional, feminine looking, with normal voiding function, satisfactory sexual function, and minimal scarring. Ideally, the neovagina should be moist, flexible and hairless, and a minimum of 10 cm in depth and 3-4 cm in diameter.
The two most widespread techniques of creating neovagina are the penile inversion and recto-sigmoid procedure.
Penile inversion vaginoplasty
During the penile inversion procedure skin from the shaft of the penis is used to create a vaginal canal. Skin from the scrotum is used for labiaplasty (creating the labia). During clitoroplasty (creating a clitoris), a part of glans of the penis and neurovascular bundle that supply it are used (Figure 3). Removal of penile corpora cavernosa is performed during the procedure. In a case of insufficient penile skin scrotal skin flaps can also be used to create a vagina. In most cases orchiectomy is done during vaginoplasty.
Penile inversion vaginoplasty is considered as the gold standard of male-to-female gender reassignment surgery which results in an authentic appearance with excellent depth, function and sensation. Postoperative use of vaginal dilators for at least 6 months is required.

Figure 3 Anatomy before and after penile inversion
Sigmoid vaginoplasty
Sigmoid vaginoplasty uses a section of the sigmoid colon to create the neovagina, if there is not enough penile and scrotal skin for the penile inversion method (Figure 4). Removal of penile corpora cavernosa and reduction of glans are performed simultaneously. Sigmoid vaginoplasty can be used also as a salvage procedure after failed penile inversion vaginoplasty.
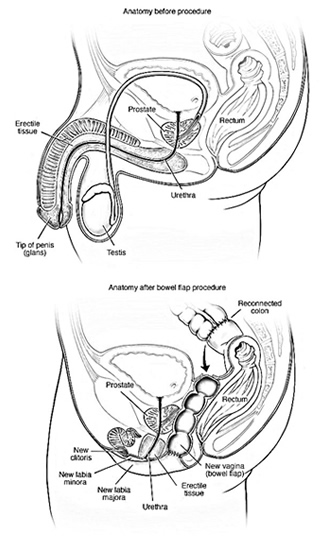
Figure 4 Anatomy before and after bowel flap procedure
Sigmoid vaginoplasty is a much more invasive surgery, it requires longer recovery time and carries the higher risk of serious complications, like rectal fistula. The self-lubricating quality of the sigmoid colon graft is good. The sigmoid graft created neovagina is unlikely to provide the quality of sensation obtained with penile inversion. Complications can include colitis, vaginal atrophy, and constipation. In most cases orchiectomy is done during vaginoplasty.
After vaginoplasty
After vaginoplasty a catheter placed in urethra is needed to collect urine. Vaginal dilatations, by timely inserting a vaginal dilators of increasing sizes, or penetrative intercourse are necessary in order to maintain, lengthen and stretch the size of neovagina. Recovery can take up to two months. Doctor will provide instructions about when to begin with sexual activity.
Because the prostate gland is not removed during surgery prostate cancer screening is necessary.
Complications of feminizing surgery
Surgical complications of MtF genital surgery may include complete or partial necrosis of the vagina and labia, fistulas (an abnormal connection between two body parts) from the bladder or bowel into the vagina, stenosis of the urethra and vaginas that are either too short or too small for coitus. While the surgical techniques for creating a neovagina are functionally and aesthetically excellent, anorgasmia (loss of sexual pleasure and functioning) following the procedure has been reported. Other complications are: a risk of bleeding, infection and an adverse reaction to anesthesia, poor wound healing, seroma (accumulation of fluid beneath the skin), hematoma (solid swelling of clotted blood within tissues), changes in skin sensation (persistent pain, tingling, reduced sensation), tissue necrosis (dead body tissue), deep vein thrombosis or pulmonary embolism (a blood clot in a deep vein or in a lung), dissatisfaction with appearance after surgery.
Lower urinary tract infections occur frequently in these patients who have had surgery due to the shortened urethra. These patients may suffer from functional disorders of the lower urinary tract caused by damage of the autonomous nerve supply of the bladder floor during dissection between the rectum and the bladder. A dysfunctional bladder (overactive bladder, stress or urge urinary incontinence) may occur after gender affirming surgery.
Gender affirming surgical procedures significantly improve quality of life and reduce the symptoms of gender dysphoria, with low rates of regret following these gender affirming surgeries. Even patients who develop severe surgical complications seldom regret having undergone surgery.
All these procedures are performed according to WPATH Standards of Care.
POSTOPERATIVE CARE AND FOLLOW-UP
Long-term postoperative care and follow-up after surgical treatments for gender dysphoria is important to a patient’s physical and mental health and to a surgeon’s knowledge about the benefits and limitations of surgery. Surgeons who operate on patients coming from long distances should ensure personal and regular follow-up and long-term aftercare.
The need for follow-up equally extends to mental health professionals who have spent a longer period of time with the patient than any other specialist and therefore are in position to assist in any postoperative adjustment difficulties.
Transgender people need health care throughout all their lives. To avoid the negative effects of undertaken treatment in a form of receiving long-term, high-dose hormone therapy and top and bottom surgery patients need thorough medical care by doctors experienced in primary care and transgender health. If one doctor is not able to provide all services ongoing communication among specialists is essential. While endocrinologists and surgeons play important roles in preventive care, every transgender person should have a primary care doctor for overall health care needs. These patients receiving hormone therapy and having surgery need regular checkups and screenings for cardiovascular risk factors, osteoporosis and some cancers (breast, cervical, ovarian, uterine and prostate).
All transgender patients should receive counseling regarding genital hygiene, sexuality and prevention of sexually transmitted infections.
Source used: Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, The World Professional Association for Transgender Health (WPATH), (https://www.wpath.org/publications/soc)

