Undescended testes (Cryptorchidism)
What is undescended testes (Cryptorchidism)
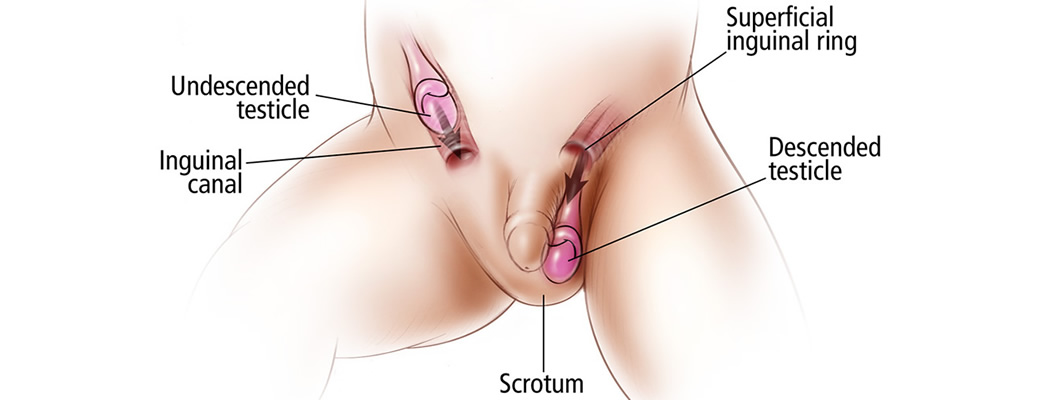
It is a condition in newborns when one or both testes have not moved into their proper position in the scrotum before birth. About 1 in 10 cases affect both testes. Undescended testes are more often seen in babies who are born early (premature babies).
Cryptorchidism often corrects itself within a six months of birth. After that period an infant needs surgery to relocate the testicle to the scrotum.
How to diagnose an undescended testes?
An undescended testicle is typically detected when your baby is examined shortly after birth by clinical examination, palpation, when it is seen that the scrotum is empty. In the most cases the testis is palpated in the inguinal canal. If the testicle isn’t present in the scrotum and can’t be palpated in the inguinal canal it is necessary to do the ultrasound imaging to see its position, size and structure. If the testicle hasn’t moves into the scrotum by the time your son is 6 months old, the problem probably won’t correct itself.

What is a “retractile” testicle?
Older boys, who had normally descended testicles at birth can appear to be ‘missing’ a testicle later. It can be due to a “retractile testicle”, this is not abnormal and it is due to a muscle reflex in the scrotum.
You need to see the doctor if You detect that the scrotum is empty. The doctor will decide if it is a classic case of undescended testes or is it the retractile testes and will continue to monitor the condition. A retractile testicle is present in the scrotum most of the time. If the testicle is present more in the inguinal canal than the doctor will consider surgery. Occasionally, ultrasound examines the size of the testicle and identifies possible asymmetry in size that would indicate a stalled growth. In this case, surgical treatment or testicular fixation in the scrotum is advised.
A retractile testicle and might be easily guided by hand into the scrotum during a physical exam. This condition usually doesn’t require surgery since as the kid grows the testicle will get in the scrotum where it should be.
How to diagnose undescended testes?
The most common sign is when the doctor can't feel the testes during an exam. The testicle is usually located at the end of the inguinal canal, a channel that carries the spermatic cord towards the penis and scrotum. If a doctor cannot feel the undescended testicle further diagnostics is needed.
True undescended testes cannot be easily guided into the scrotum and the testicle is usually palpated in the inguinal canal.
The doctor inserts a tiny tube with an attached camera through the incision made in the abdomen. Orchidopexy can be done in the some act.
If there is no testes found during laparoscopy the diagnoses is called absent testes.
What are the complications of undescended testes?
If the testicle is not surgically put in place and fixed into the scrotum, there will be damage to the germ cells that lead to impaired fertility-infertility, especially if both testicles are not lowered. Untreated testicle carries an increased risk of developing a malignant tumor.
The child may have psychological and psychosexual problems due to an empty scrotum.
When and how do you treat undescended testes?
The only treatment for undescended testes is surgery. The surgery is called orchidopexy and the ideal time for doing it is when the boy is between 6 and 18 months old.
How is the surgery-orchidopexy being done?
An undescended testicle is usually corrected with surgery- Orchidopexy. The aim of the operation is to place the testicle in the scrotum and prevent the possibility of developing complications.
The child is put he child is put under (general anesthesia) for this surgery. The child needs to be healthy before surgery to avoid the risk of anesthesia-related complications. A cut about 1 inch long is made in the groin area (most often it can hardly be seen later).The testicles is freed from all nearby tissues so that it moves easily into the scrotum. Then the path to the scrotum is made and the testicle descends into the scrotum through the canal. The canal is places under the skin. Then the testicle is stitched into place in the scrotum. Stitches that dissolve on their own will be placed under the skin to make sure that the testicle doesn’t pull back up. The incision will be covered by a simple dressing that you will be told when and how to change. If there is an inguinal hernia present the doctor will fix it in the same act.
The surgery will take about 45 minutes.
Laparoscopic surgery for undescended testes?
If the testicle is not identified by ultrasound either in the inguinal canal or in the scrotum before surgery, it is likely to be high in the abdomen. The laparoscopic procedure is then indicated when the camera enters the abdomen under general anesthesia and the abdominal position of the testicle is definitely confirmed. If the testicle is seen in the abdominal cavity, the operation of positioning the testicle in the scrotum is being done immediately. If the testicle is not visible in the abdominal cavity a definitive diagnosis of absence of testicle (testicular agenesis) is made. In these cases, when the child has no testicles at all (testicular agenesis), insertion of the testicular prosthesis into the scrotum is indicated.
How long does it take to recover from the surgery?
Almost always the child can go home the same day, after normal fluid and solid food intake has been established, if the child does not vomit and is completely “awakened” from anesthesia. The child gets the medication for the pain.
Check-up appointments usually consist of examining the testicles and are every two or three days until the wound is healed. After that the check-up appointments consist of ultrasound imaging of the testicle.
After one month the child can resume with normal activities.
