Urinary incontinence

What is urinary incontinence
Incontinence is defined as any involuntary leakage of urine from the bladder.
Bladder control and normal urinary continence require a complex interaction between the brain, nervous system and organs in the pelvis. Two valves, or sphincters, are in control of the outflow of urine. They are located in the bladder neck and earliest portion of the urethra.
The bladder has two essential functions: to store and to empty urine. Perceptions of bladder filling and fullness, and following initiation of emptying requires synchronization between the nervous system, the bladder muscle, sphincters and pelvic floor.
Types of urinary incontinence
- Stress incontinence- this occurs because passive bladder pressure exceeds the urethral pressure, due to either poor pelvic floor support or a weak urethral sphincter. The presentation is with incontinence during sneezing, coughing, or exertion. This type of incontinence is the most common and occurs in women after difficult childbirth and in men after prostate surgery.
- Urge incontinence- this usually occurs because of detrusor over activity, which produces an increased bladder pressure that overcomes the urethral sphincter. It is usually idiopathic, or it can be neurogenic as in patients with spina bifida or multiple sclerosis. It is characterized by spontaneous and uncontrolled urine leakage, often accompanied by the overwhelming sensation of needing to void.
- Continual incontinence- this is suggestive of a fistula, usually between the bladder and vagina, or the ureter and vagina.
- Overflow incontinence- This results from failure of the bladder to empty either from intrinsic weakness, nerve injury or blockage to the flow. With an overfull bladder, exertion or abdominal pressure can cause urine to spill out.
What are the symptoms of urinary incontinence?
Many people experience occasional, minor leaks of urine. Others may lose small to moderate amounts of urine more frequently.
- Urine leaks when you exert pressure on your bladder by coughing, sneezing, laughing, exercising or even lifting something heavy.
- You experience frequent or constant dribbling of urine because your bladder doesn’t empty completely.
- You may need to urinate often, sometimes throughout the night.
When to seek medical help?
See your doctor if you have any type of urinary incontinence. It is a common problem and you shouldn’t feel embarrassed talking about your symptoms. Your doctor may also suggest you keep a diary in which you note how much fluid you drink and how often you have to urinate. Bladder problems could affect your quality of life and cause other health problems.
Health problems and lifestyle factors
Certain health problems can lead to urinary incontinence: aging, bladder infection, constipation, birth defects, blocked urinary tract, prostate problems, diabetes and overweight or obesity. As far as the lifestyle factors that make women and men more likely to develop UI include eating habits, for example food that causes constipation, drinking alcohol or caffeinated or carbonated beverages, certain medicines, physical inactivity and smoking.
How to diagnose urinary incontinence?
In order to determine the type and degree of incontinence, a clinical examination and clinical tests are performed as well as the urine and urinoculture analyzes. Urodynamic examination and urethroscopy are also done. If necessary, consultations are carried out by doctors of other specialties (neurologist, gynecologist, special physical medicine, etc.).
How to treat urinary incontinence?
Your doctor is likely to suggest the least invasive treatment first and move on to other options only if these techniques fail. The type of treatment depends mostly on the type and the degree of incontinence. For stress incontinence, conservative treatment involves the use of exercises to strengthen the pelvic floor muscles (Kegel exercises). In case of failure or if there is a high degree of incontinence, surgical treatment (implantation of “sling” or “sphincter”) is indicated. Implantation of the so-called “bulking material” into the sphincter for better closure of the sphincter generally has no satisfactory effect.
Other types of incontinence (urge incontinence) can be treated: so-called biofeedback and behavioral therapy (bladder training, planned urination, planned fluid intake and diet), using medication (anticholinergics, alpha-blockers, topical estrogens). If neurological damage is causing urinary incontinence, electrical stimulation is applied (installing a pacemaker-like device under the skin to send painless nerve impulses to the nerves and thereby participate in control of urination), or administration of botox injections into the bladder muscle in people with hyperactive bladder.
-Sling procedures - are used to treat stress incontinence, mainly in women, who have muscle weakness after difficult childbirth. Sling is a band that is placed around the urethra during surgery and then tightened until satisfactory degree of continence is reached. Sling installation surgery may also be indicated in men who have mild or moderate incontinence.
-Artificial urinary sphincter - this method represents the "gold" standard in treat stress incontinence.
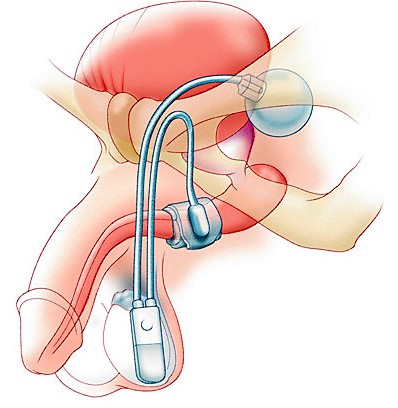
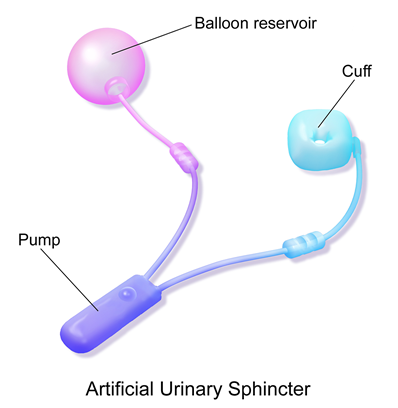

 The device has 3 main components attached to each other: the cuff (surrounding the urethra), the pump (placed in the scrotum next to one of the testes) and the reservoir (placed in the pelvis).
The device has 3 main components attached to each other: the cuff (surrounding the urethra), the pump (placed in the scrotum next to one of the testes) and the reservoir (placed in the pelvis).
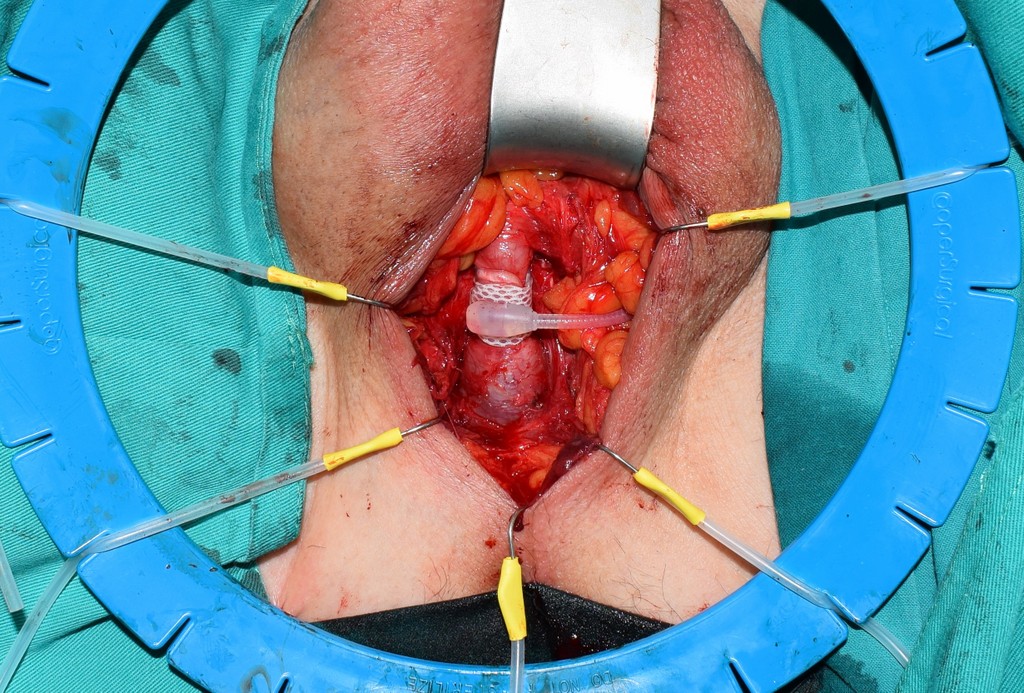
- The procedure is usually carried out under a general anesthesia.
- An incision is made in your perineum (the area between the back of the scrotum and the anus); if the cuff is being inserted at the bladder neck, the incision will be in your lower abdomen (tummy). Your urethra is being mobilized and the cuff is positioned around your water pipe. Another small incision in the abdomen is made to implant the balloon and to pass the control pump down into the scrotum. The components are connected with tubing and are filled with sterile fluid. Your skin incisions are closed with dissolvable stitches.
- A catheter is placed in your bladder during the operation; this may be removed before you wake up or on the following day (before your discharge from hospital) . You will stay in hospital for 1 or 2 days after the surgery.
- Leading studies show that patients are very satisfied and that about 90% of patients undergoing this procedure would suggest the same procedure for their friends or family members suffering from the same disease.
- After the sphincter is installed, the patient receives a guarantee for the sphincter and a document stating when and what type of the sphincter is installed, as well as the name of the physician who performed the surgery.
After recovering from surgery, the patient is trained how to use the artificial sphincter. In the normal resting mode, the cuff is full of water, compressing the urethra. When the patient feels his bladder is full, he goes to the toilet and squeezes the pump, which opens the cuff, allowing urine to drain out. Over the next 2-3 minutes the cuff automatically re-fills, closing the urethra again.
Many people are embarrassed about a bladder control problem but effective treatments are available for urinary incontinence. It is important to ask your doctor about the best treatment for you.